Background
A 32-year-old female presented with a sacral mass. PET-CT showed a metabolically active lobulated soft tissue mass measuring 10.5 x 5 cm, in the presacral region and involving adjacent gluteal muscles. Incisional biopsy was obtained.
Microscopy

Fig.10a; H&E; 5x
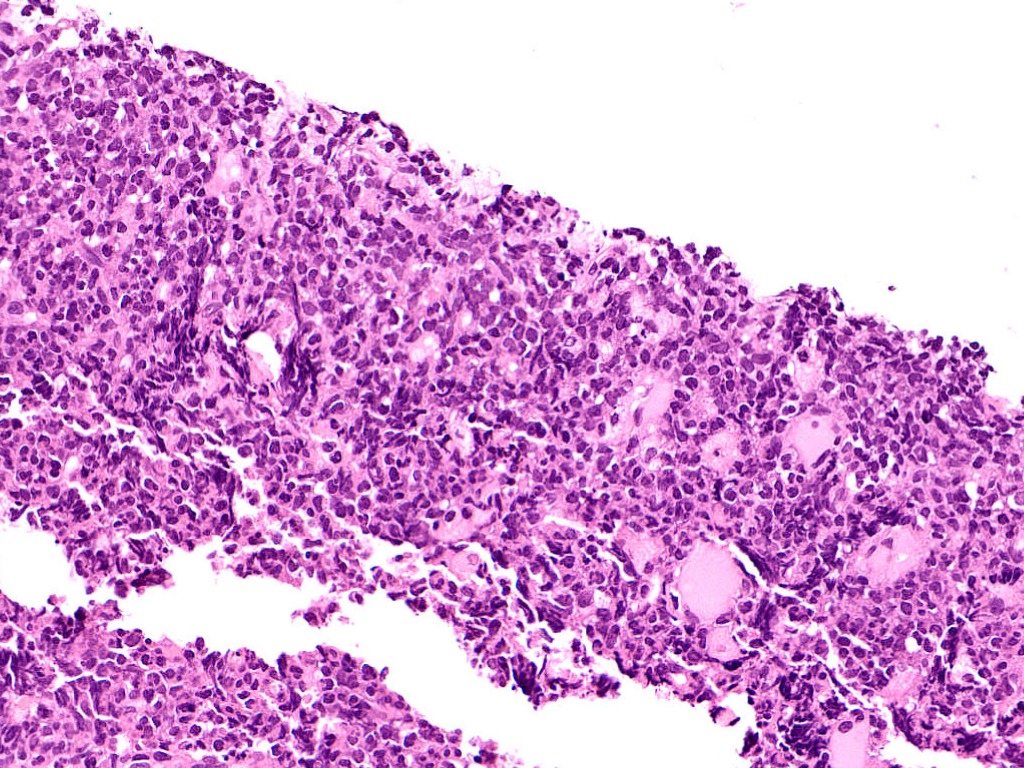
Fig.10b; H&E; 20x

Fig.10c; H&E; 20x

Fig.10d; H&E; 10x
Images show a high grade round cell tumor in sheets. The tumor cells have hyperchromatic nuclei and scant cytoplasm [Fig.10a-b]. Brisk mitosis and apoptosis is evident [Fig.10c]. Areas of necrosis also seen [Fig.10d].
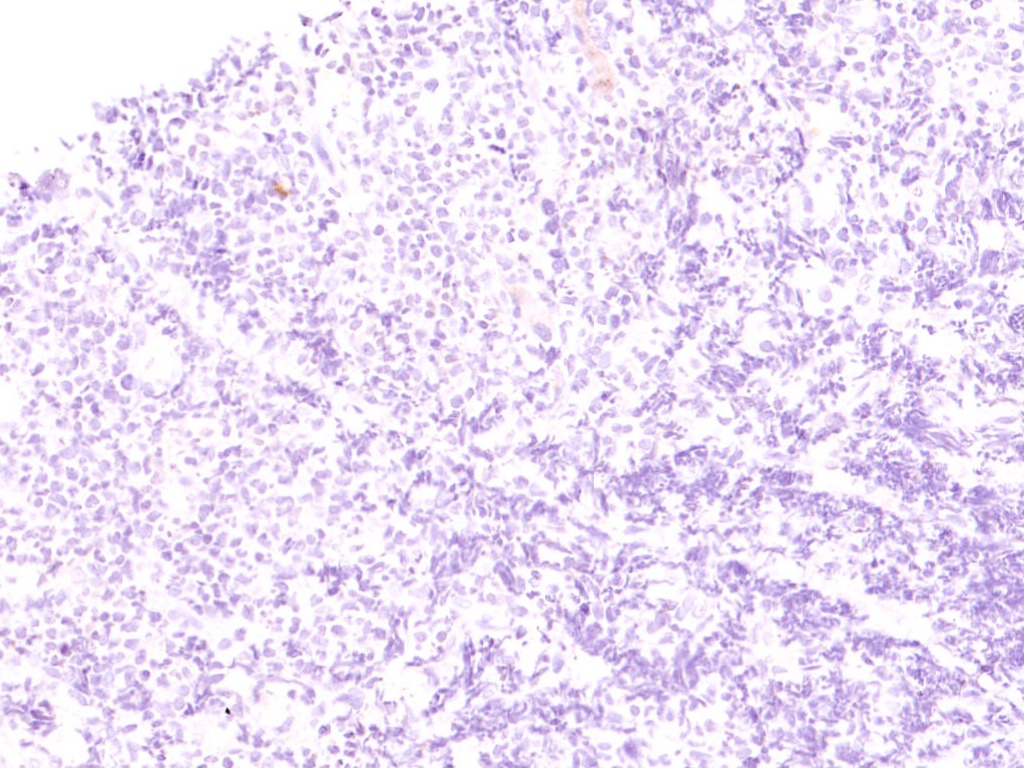
Fig.10e; CK
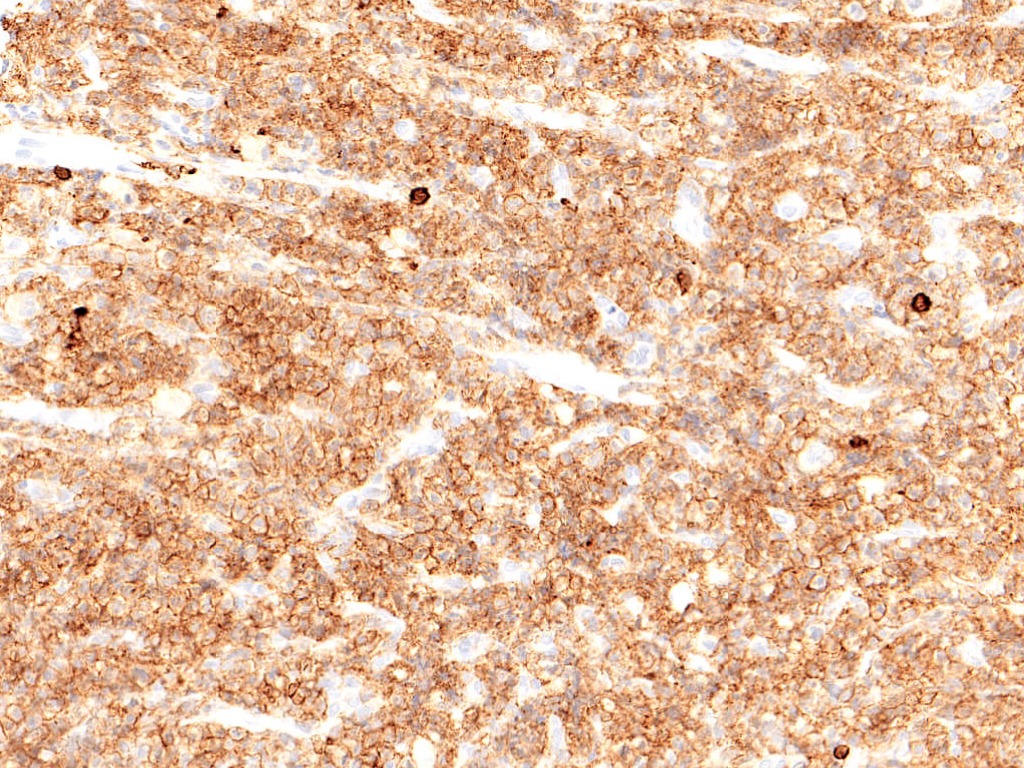
Fig.10f; LCA

Fig.10g; CD20
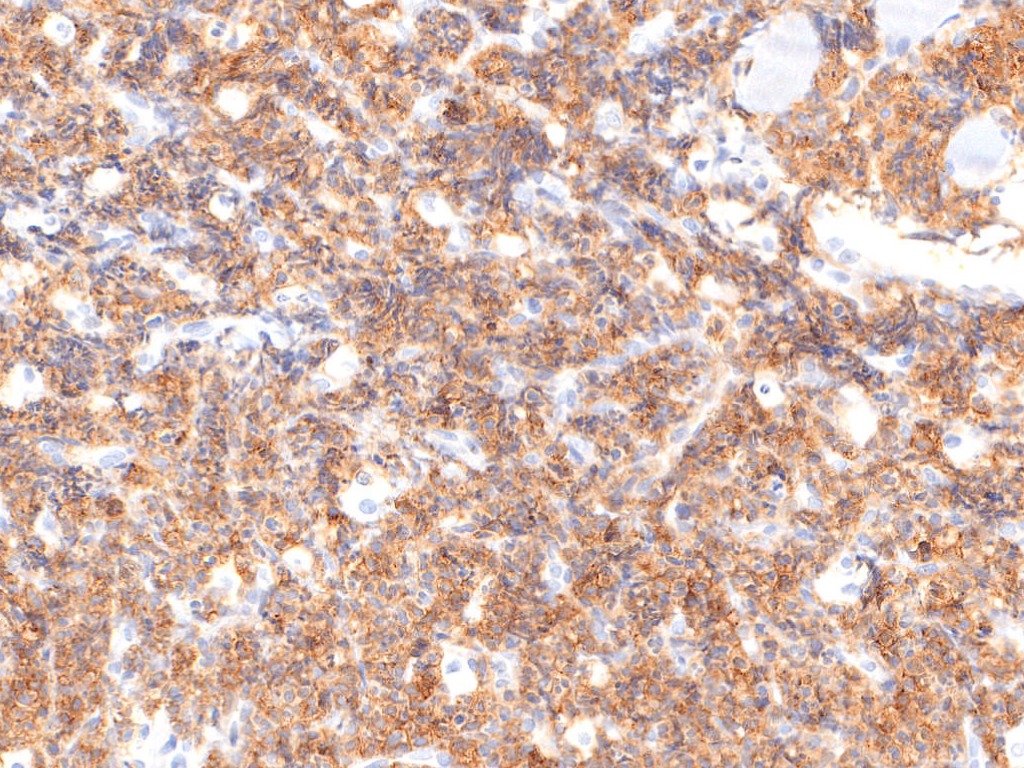
Fig.10h; CD117
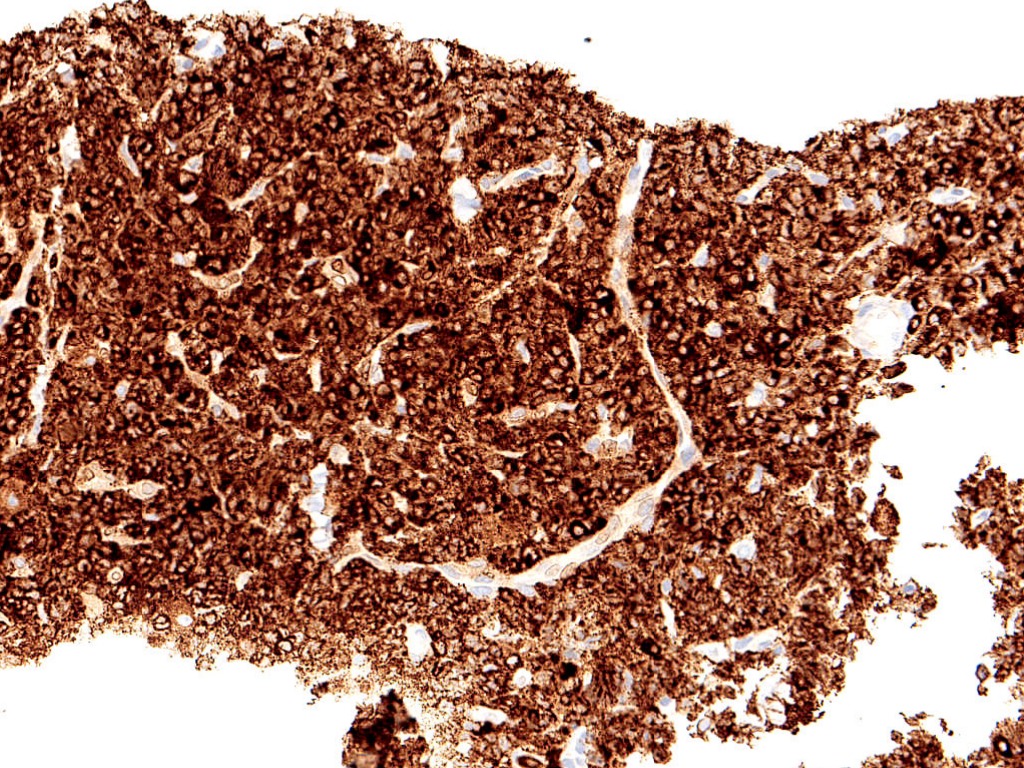
Fig.10i; MPO
Immunohistochemistry reveals tumor cells are negative for CK [Fig.10e], while are positive for LCA [Fig.10f]. On further IHC, these cells are negative for CD3 and CD20 [Fig.10g]. Diffuse CD117 & MPO positivity is noted in tumor cells [Fig.10h-i].
Final Impression: Myeloid Sarcoma.
- Definition:
- A myeloid sarcoma is a tumor mass consisting of myeloid blasts, with or without maturation, occurring at an anatomical site other than the bone marrow.
- However, infiltration of myeloid blasts in a patient with leukaemia is not classified as myeloid sarcoma unless it presents with tumour masses in which the tissue architecture is effaced.
- Synonym: Chloromas (due to a greenish color of the tissues imparted by myeloperoxidase present in the cytoplasm of tumor cells).
- Age of presentation: Wide range (from one month to 89 years)
- Common sites of involvement include skin, lymph nodes, gastrointestinal tract, bone, soft tissue, and testes.
- It may precede or coincide with acute myeloid leukemia or constitute acute blastic transformation of MDS, myelodysplastic/ myeloproliferative neoplasms (MDS/MPNs), or MPN.
- Pathogenesis: believed to be an aberrant expression of homing signals for the leukemic blasts on extramedullary sites as compared to bone marrow.
- Microscopically: Myeloid sarcoma most commonly consists of myeloblasts with or without features of promyelocytic or neutrophilic maturation. In a significant proportion of cases, it displays myelomonocytic or pure monoblastic morphology.
- Immunohistochemistry:
- Positive stains: CD33, CD34, CD68, and CD117.
- Staining for TdT, MPO, and C045 is variable.
- Genetic profile:
- Monosomy 7, trisomy 8, KMT2A rearrangement, inversion (16)
- Trisomy 4, monosomy 1, loss of 16q, 5q, or 20q, trisomy 11 and NPM1 mutations.
- Prognosis : Clinical behaviour and response to therapy do not seem to be influenced by age, sex, anatomical site involved and type of presentation.
Contributed by: Dr. Anila Sharma
Compiled by: Dr. Akanksha Malik
In case of queries, email us at: kumar.ankur@rgcirc.org
Hematolymphoid neoplasm MPO Myeloid sarcoma
Last modified: 05/06/2021








