Background
A 36-year-old female presented with menorrhagia and abdominal pain. CECT revealed a right sided large enhancing mass in the pelvis measuring 12.8cm in size. Serum CA-125: 30.3U/ml. Patient underwent debulking surgery. Sections from ovary for examination.
Microscopy
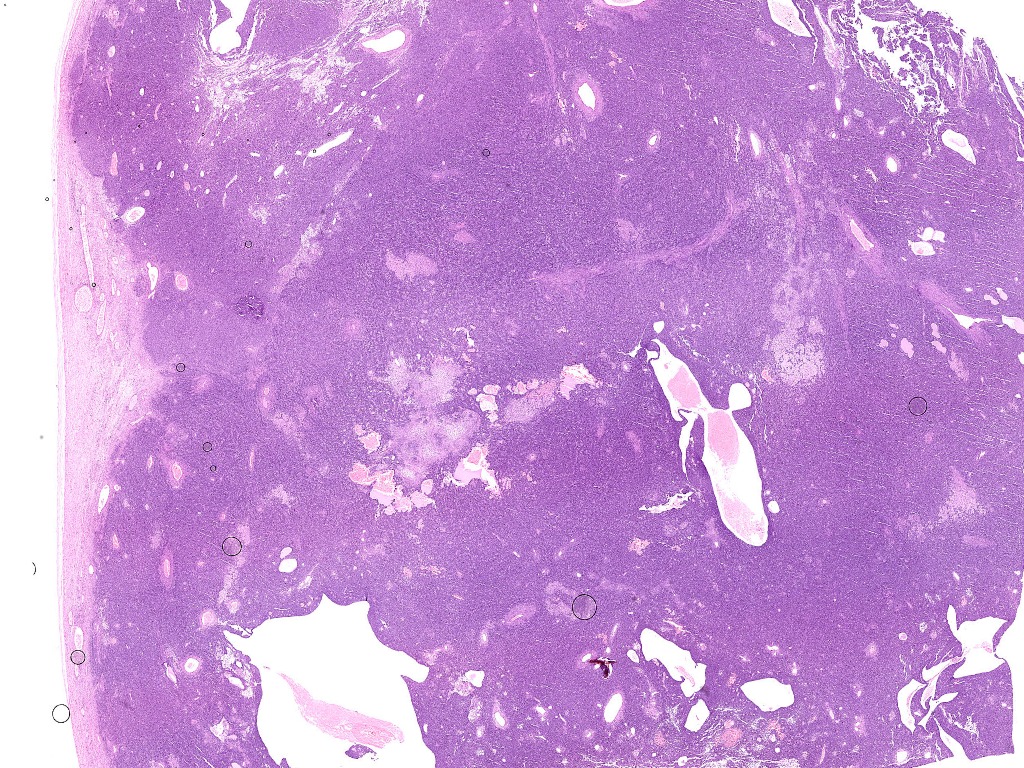
Fig.9a; H&E; 0.38x
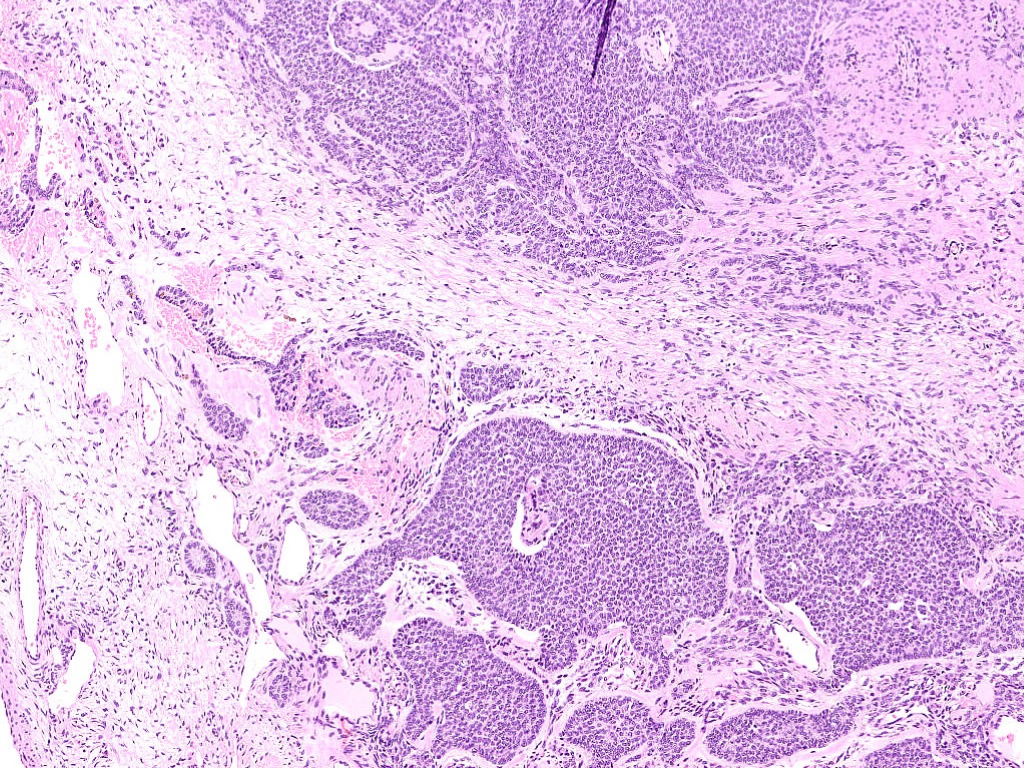
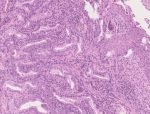
Fig.9b; H&E; 5x
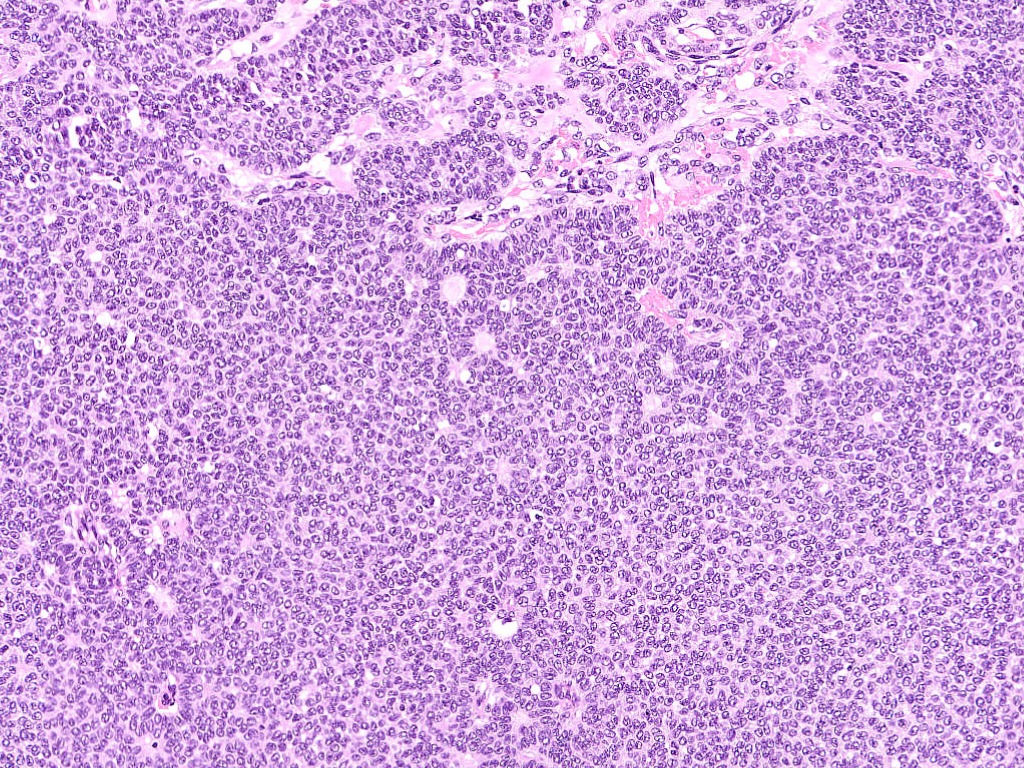
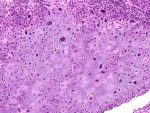
Fig.9c; H&E; 10x
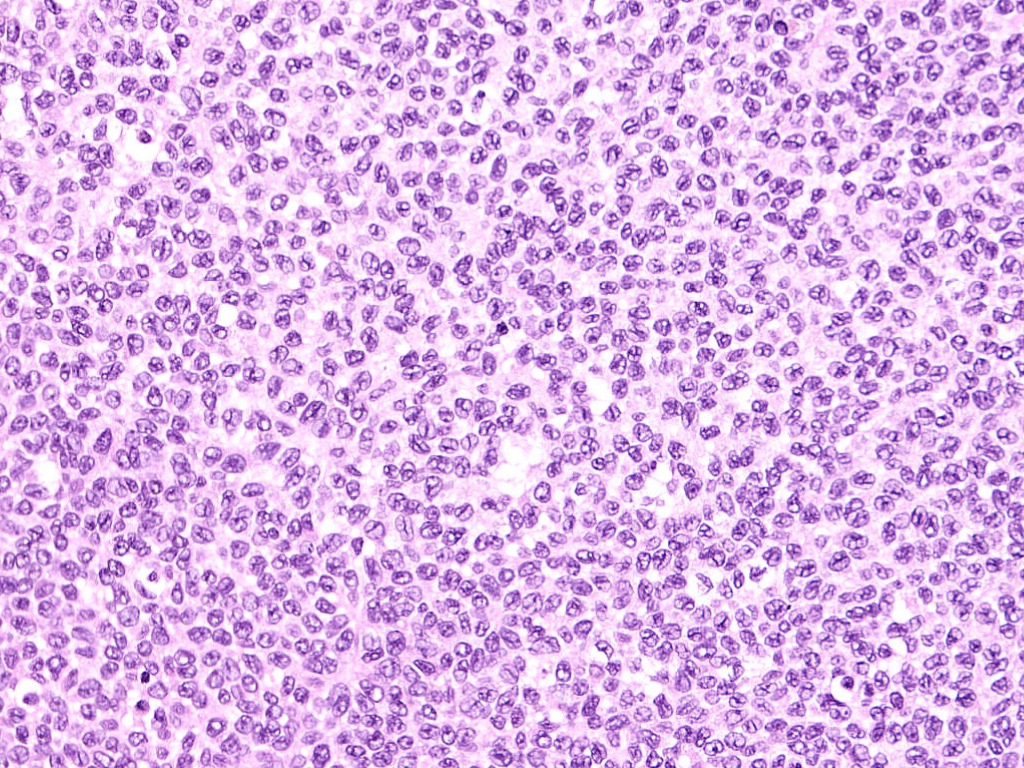
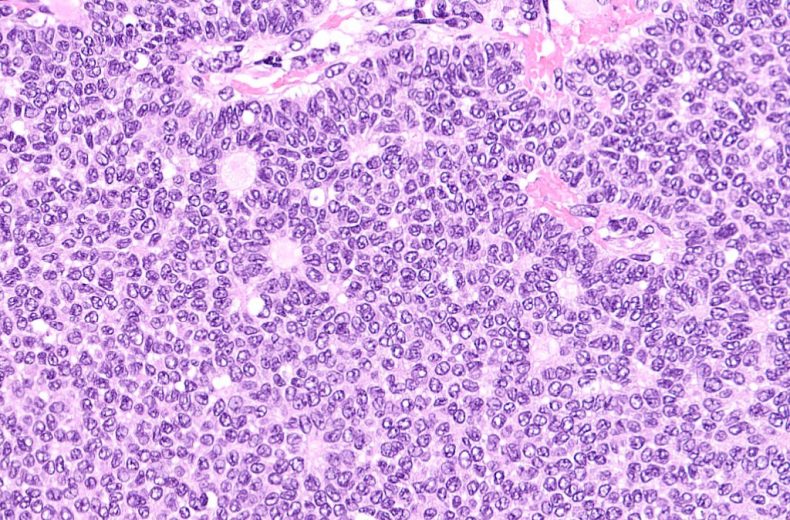
Fig.9d; H&E; 20x
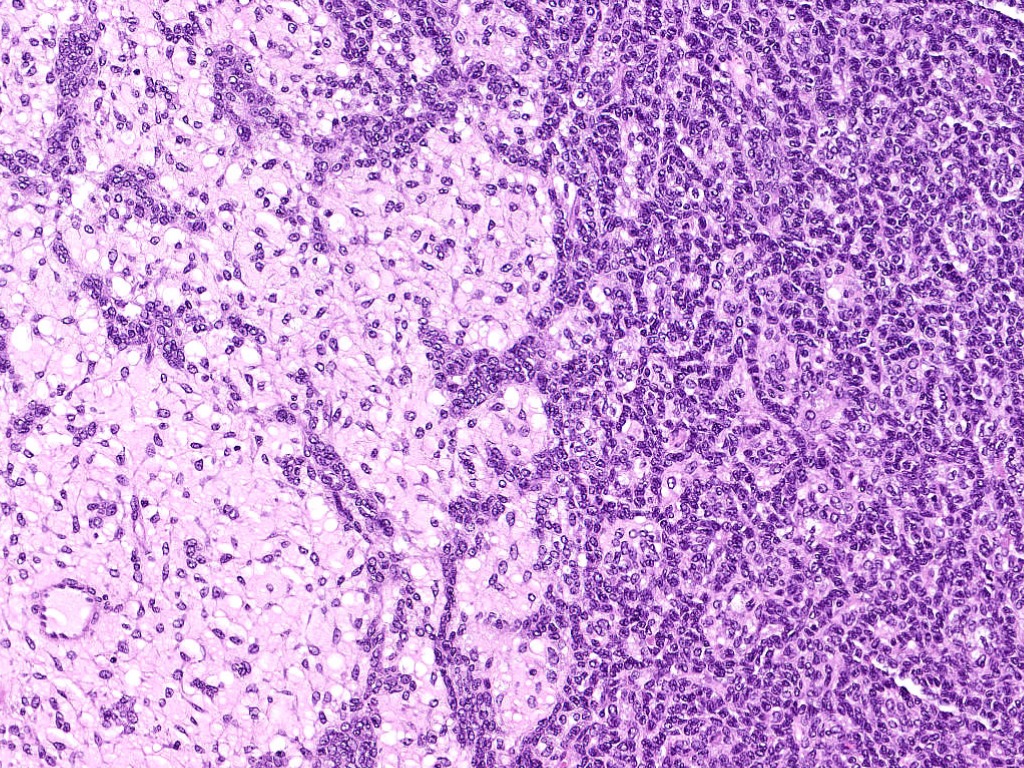
Fig.9e; H&E; 10x
Images show a tumor arranged in diffuse sheets, nests and cords [Fig.9a-b]. At foci, microfollicular pattern of arrangement of tumor cells (Call-Exner bodies) is also observed [Fig.9c]. The tumor cells are round to oval having angulated vesicular nuclei showing prominent nuclear grooves [Fig.9d]. The stroma is edematous with foci of theca cell proliferation [Fig.9e].
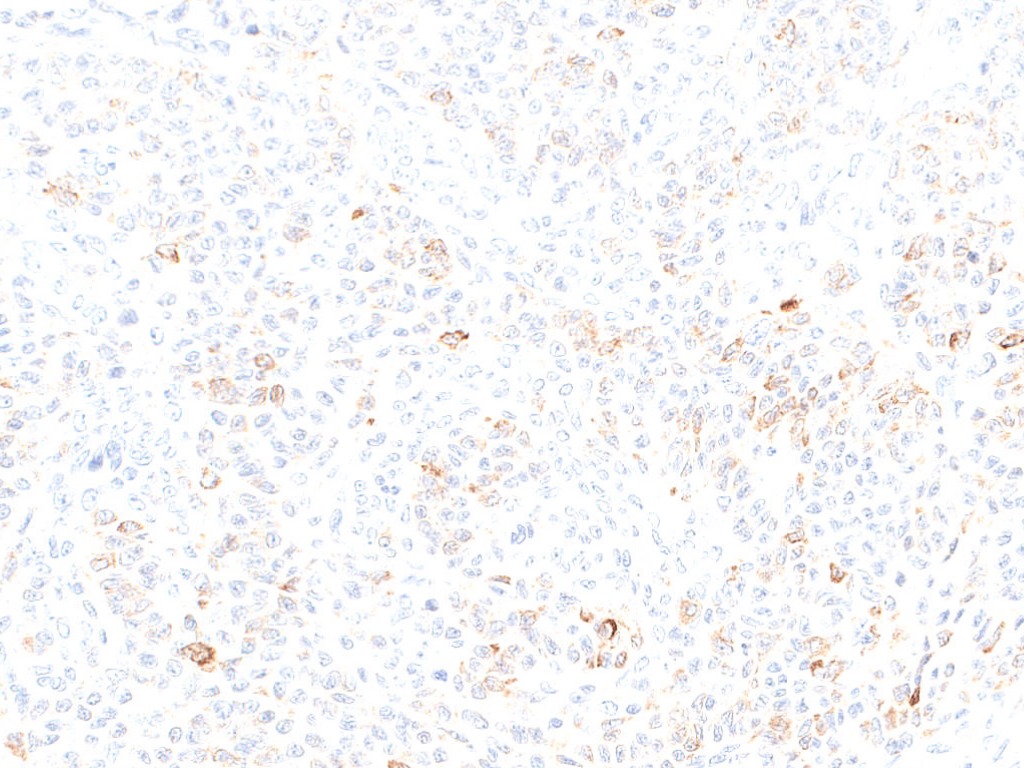
Fig.9f; Inhibin
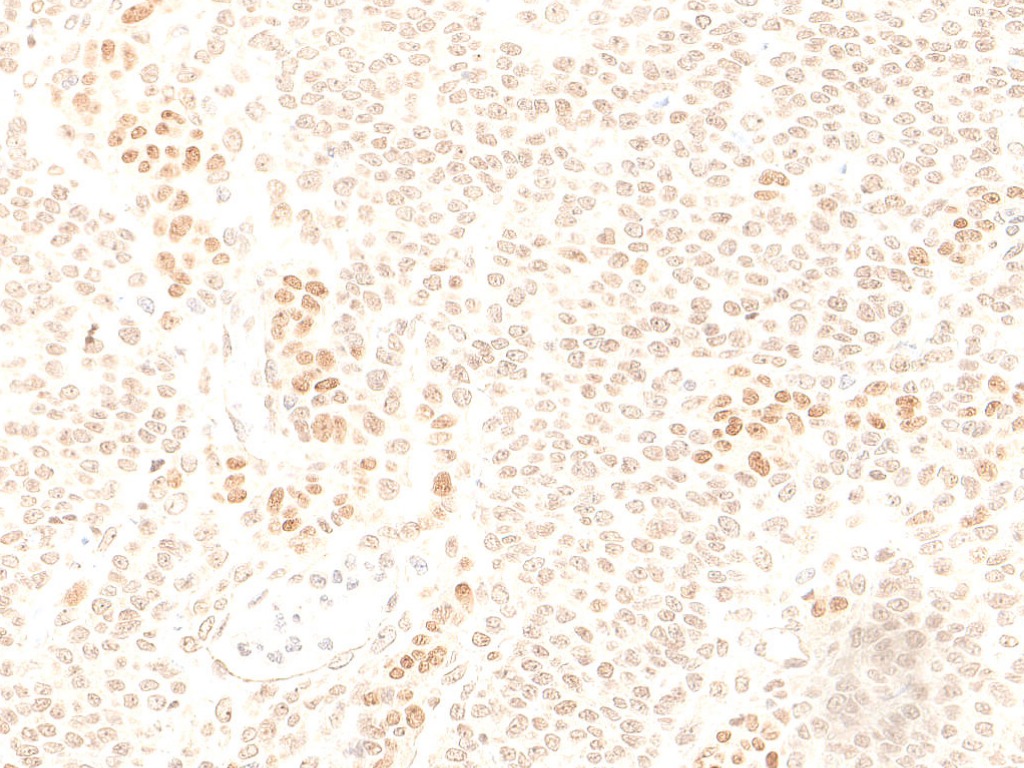
Fig.9g; SF-1
On Immunohistochemistry, tumor cells are positive for Inhibin [Fig.9f] & SF-1 [Fig.9g].
Final Impression: Adult granulosa cell tumor.
Adult Granulosa cell tumor:
- It is a low grade malignant sex cord stromal tumor composed of granulosa cells with a variable number of fibroblasts and theca cells.
- Age of presentation: Wide age range with an average age of 45 to 55 years
- Clinical presentation:
- Post-menopausal bleeding in older women
- Menorrhagia, metrorrhagia or amenorrhea in young women
- Tumor is confined to the ovary (FIGO Stage I) in 80-90% cases
- Serum Inhibin levels: markedly elevated in nearly all patients
- Gross: Typically solid and cystic gross appearance
- Microscopically:
- Mixture of several histological growth patterns can be seen.
- Microfollicular pattern (Call-Exner bodies) is the most characteristic and consists of nest and sheets of granulosa cells punctated by small spaces filled with eosinophilic secretions.
- Nuclear grooves are characteristic.
- Immunohistochemistry:
- Positive stains: Inhibin, Calretinin, FOXL2, SF-1, CD56 and WT-1
- Negative stains: CK7 and EMA
- Unfavourable prognostic factors:
- Advanced stage
- Large size (>15cm)
- Bilaterality
- Tumor rupture
- Molecular: Mis-sense somatic point mutation in FOXL2 gene (402C-G)- seen in >90% of adult granulosa cell tumors
Juvenile Granulosa cell tumor:
- Age of presentation: Children and young adults, usually in first three decades
- Clinical presentation: Isosexual pseudo precocity in young girls
- Microscopically:
- Nodular or diffuse growth pattern punctuated by follicles of varying sizes containing basophilic or eosinophilic secretions
- Nucleus lacks presence of longitudinal grooves
- Molecular:
- Most common genetic abnormality: Trisomy 12
- Absence of FOXL2 gene mutations
- Prognosis: Typically limited to ovary at diagnosis with good prognosis
- Associated syndromes :
- Olliers disease (enchondromatosis)
- Mafucci syndrome (enchondromatosis and multiple subcutaneous hemangiomas)
Contributed by: Dr. Anila Sharma
Compiled by: Dr. Ankur Kumar & Dr. Saloni Pahwa
In case of queries, email us at: kumar.ankur@rgcirc.org
Female genital tract Granulosa cell tumor Ovary
Last modified: 04/06/2021