Background
A 62-year-old male patient presented to the outpatient facility of hematology department with complaints of headache and visual disturbances. He also had history of hypertension. General physical examination revealed plethora of palms and face. Abdominal examination revealed splenomegaly. Cardiac, respiratory and central nervous systems examination were unremarkable. No lymphnodes were palpable. CBC revealed Hb – 17.5g/dl, TLC – 34,000 /cu mm, Platelet count- 9,79, 000/cu mm.
Microscopy
Peripheral smear examination shows normocytic normochromic RBC. Differential leucocyte count does not show any blasts or shift to left. Platelets are similar to machine counter.
Bone marrow aspirate- Cellular marrow trails with normal erythroid and myeloid series maturation. Megakaryocytes show pleomorphism. (M:E : 3:1)
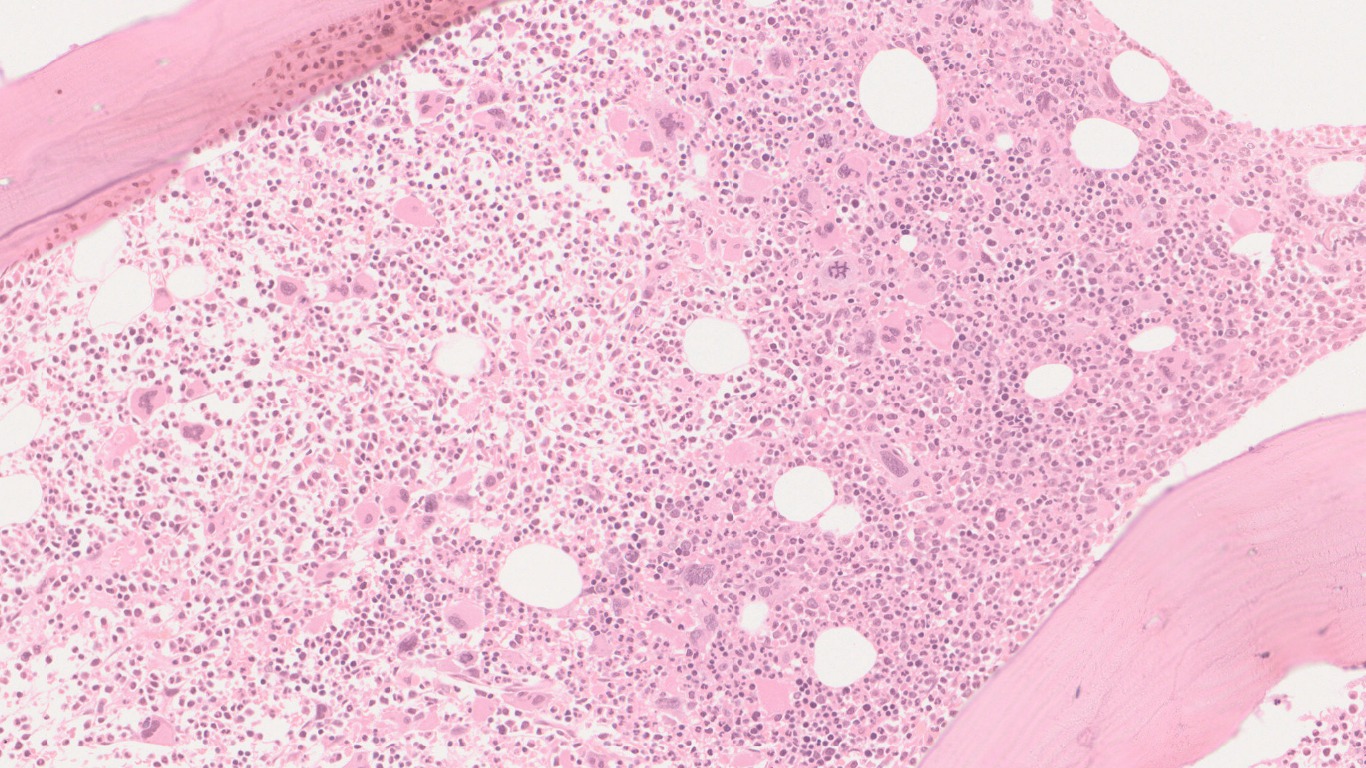
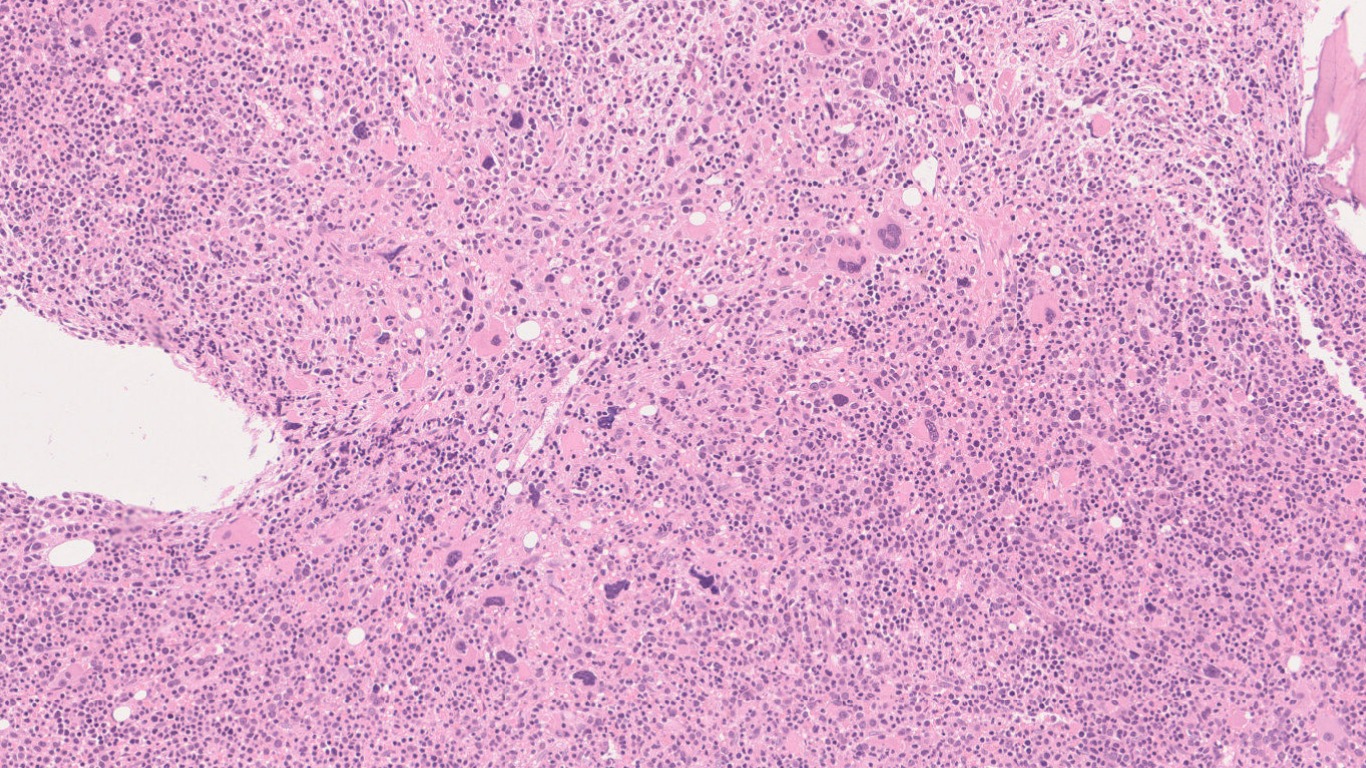
Bone marrow biopsy shows a hypercellular marrow with panmyelosis along with pleomorphic megakaryocytes. Loose clustering is noted at places. No increased immature cell clusters seen.
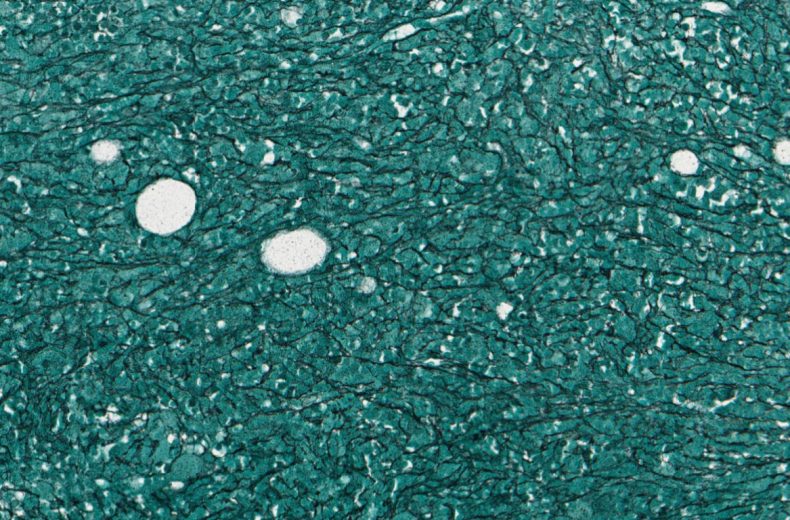
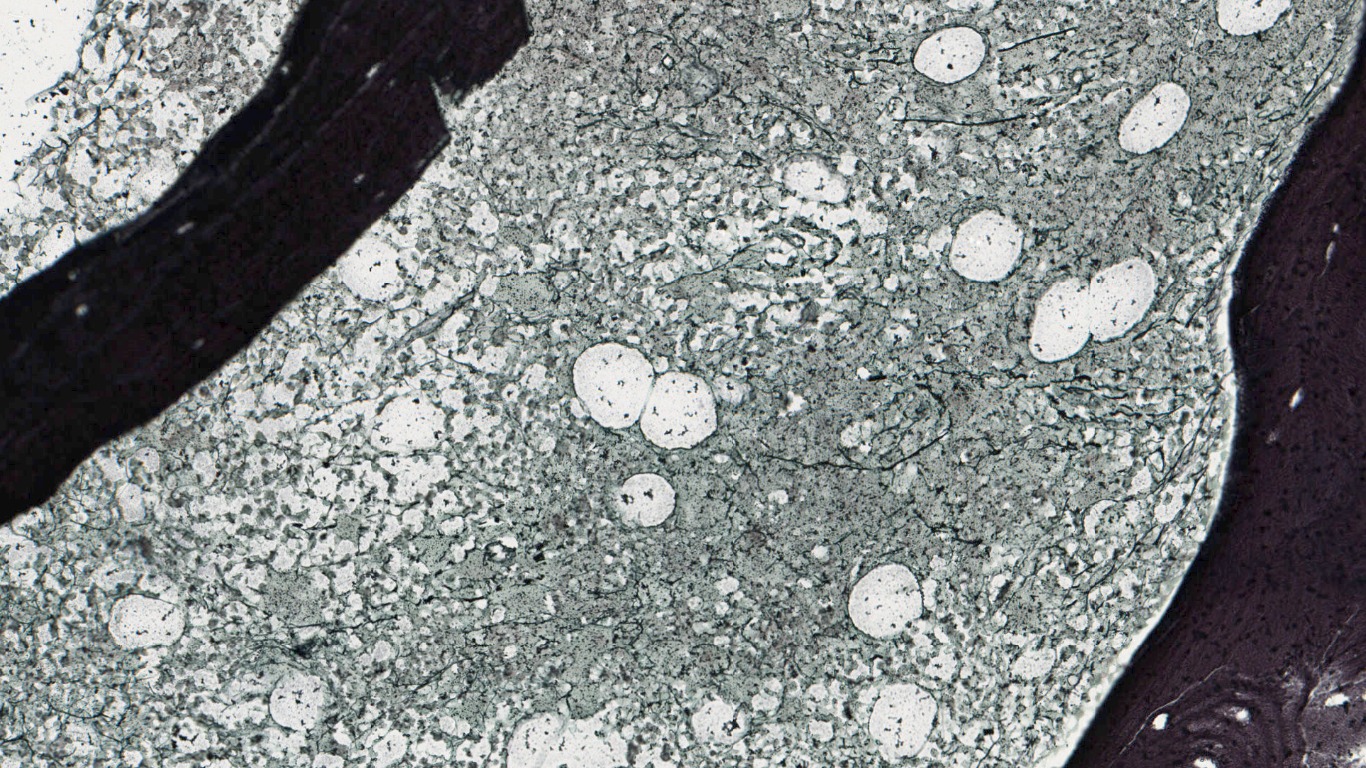
Reticulin stain shows grade 1 reticulin fibrosis.
Karyotyping was normal. JAK2 V617 mutation was detected on molecular studies.
Opinion: Polycythemia Vera (PV).
Follow-up
He presented again to the haematology OPD after three years with complaints of low grade fever and weightloss. On abdominal examination massive splenomegaly was detected. On CBC, Hb was 7.5g/dl, WBC was 27700/cumm, Platelet count was 23000/cumm.
Microscopy
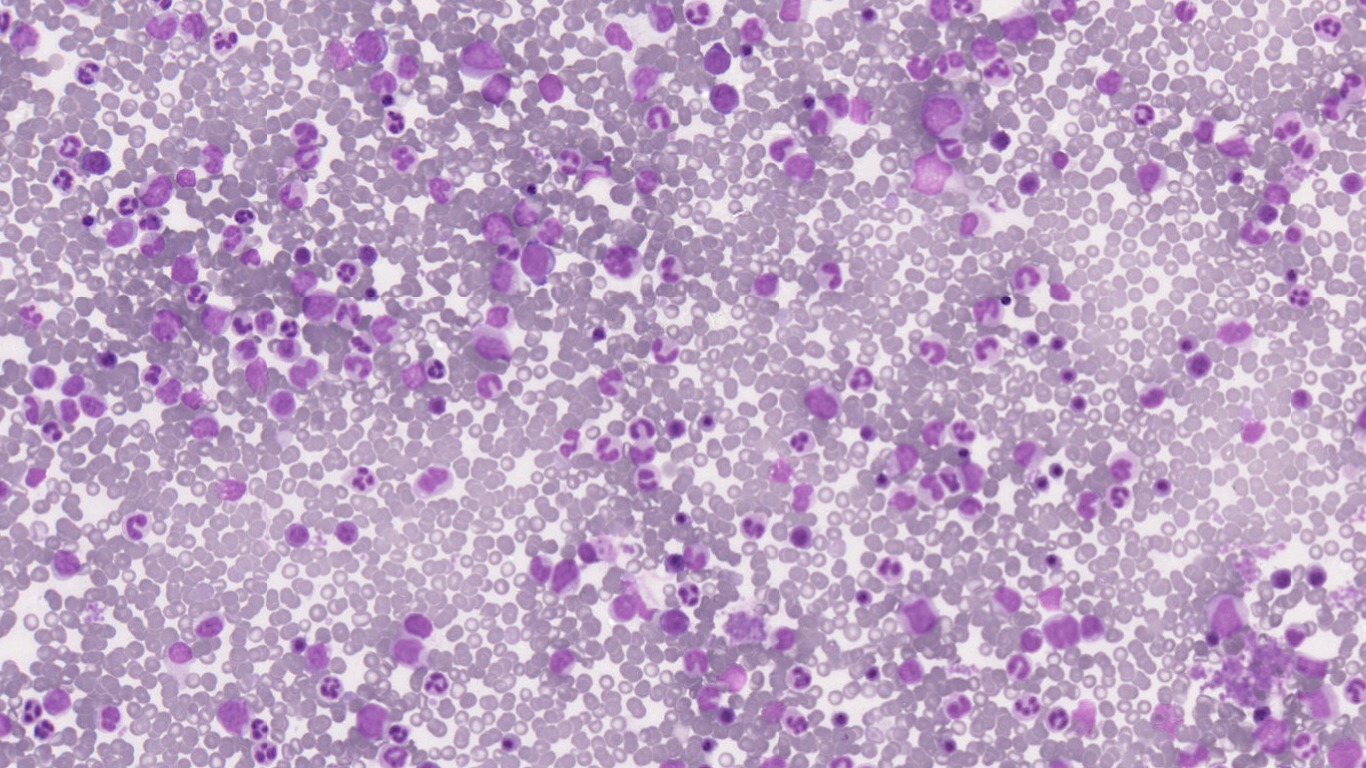
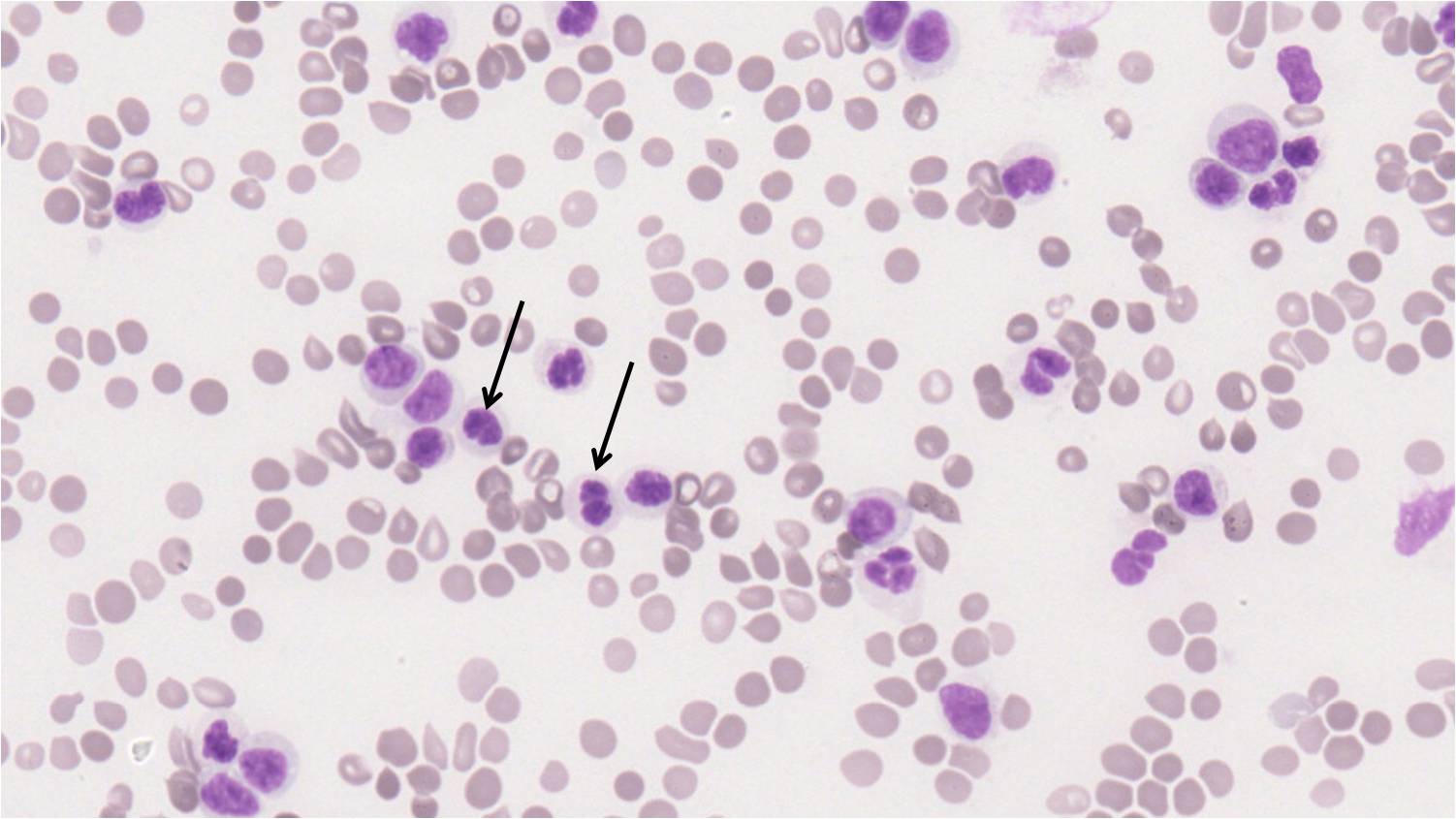
Peripheral smear shows leukocytosis with leukoerythroblastic blood picture, and presence of 13% blasts. RBC also show tear drop cells. Pseudopelger Huet neutrophils [Arrow] are also seen. Significant dysplasia was noted in the myeloid series.
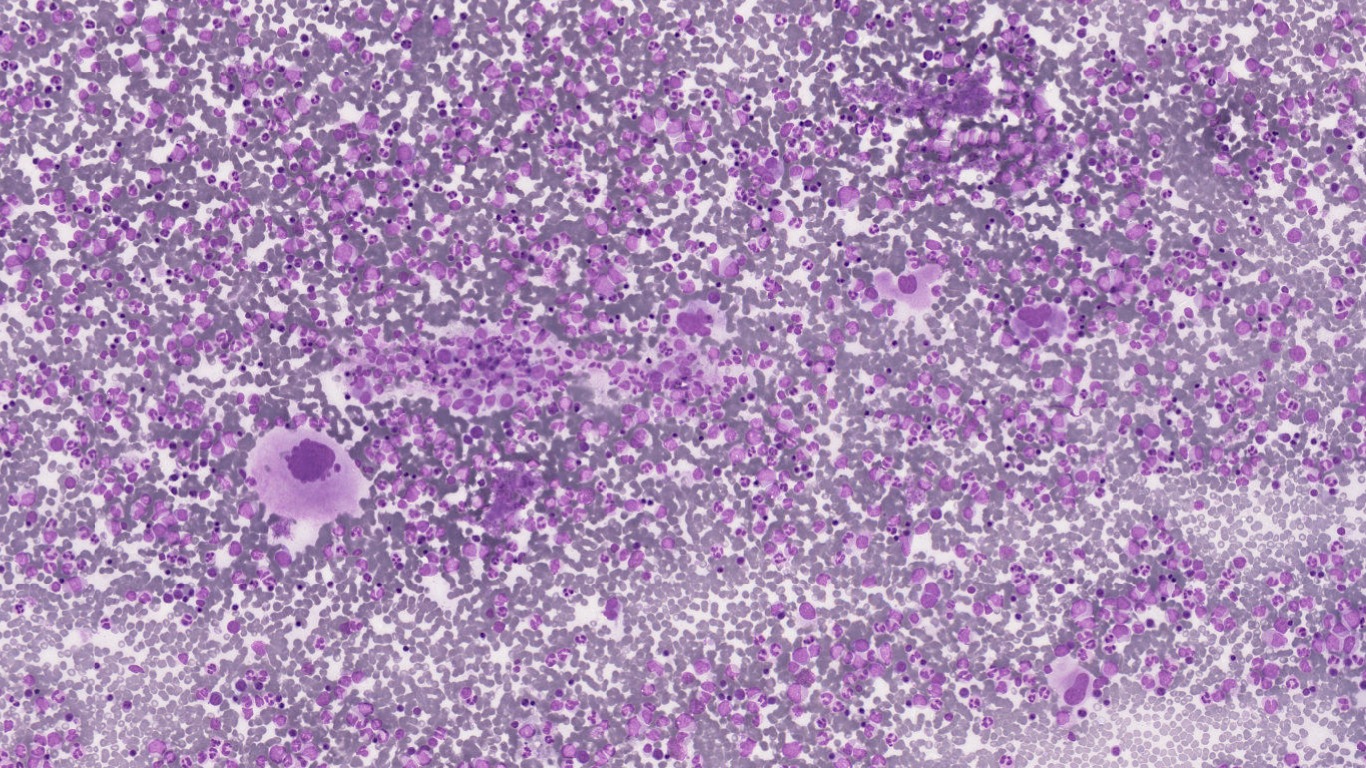
Bone marrow smears were dilute showing peripheral blood components.
Bone marrow biopsy shows a hyper cellular marrow with ~100% cellularity. There is panmyelosis, showing proliferation of all three hematopoietic series. Megakaryocytes are increased forming loose clusters focally and showing marked pleomorphism, with many hyperchromatic forms.
Reticulin stain shows diffuse grade 2 marrow fibrosis.
Karyotype: Revealed del (5q) and del (17p).
Final Diagnosis: Accelerated phase of post-Polycythemia Vera Myelofibrosis (PV-MF).
- Post-PV MF represents a natural evolution of PV.
- Less than 10% of PV patients evolve into MF within their first decade with reported incidences ranging from 2.3% to 23%.
- IWG-MRT consensus criteria:
- REQUIRED CRITERIA
- History of a World Health Organization (WHO)-diagnosed PV
- Bone marrow fibrosis grade ⩾ 2 (3-point scale) or ⩾3 (4-point scale).
- ADDITIONAL CRITERIA
- At least two of the following features must also be present:
- Anemia or sustained loss of need for phlebotomy and/or cytoreductive therapy
- Leukoerythroblastic peripheral smear
- Splenomegaly
- One or more constitutional symptoms
- REQUIRED CRITERIA
- Risk factors for post-PV MF :
- baseline bone marrow fibrosis
- JAK2V617 allele burden
- splenomegaly
- leukocytosis
- thrombocytosis (platelet count 455 × 109 /l)
- increased serum LDH
- ‘masked PV’ phenotype (display PV-characteristic BM morphology but lower hemoglobin levels than WHO criteria targets)
- During this phase, RBC mass normalizes and then decreases and spleen size progressively increases.
- Persistant leukocytosis is associated with an aggressive disease course.
- Accelerated phase post PV MF: ≥10% blasts in peripheral blood or bone marrow or myelodysplasia
- Blast phase post PV MF: > 20% blasts
- Frequency of chromosomal abnormalities is increased upto 80-90% in cases with post PV MF as opposed to PV where it is only 20%.
- Allogeneic hematopoietic stem cell transplantation is the only curative treatment for post-PV MF
- Survival of patients with PV was significantly worsened after progression to post-PV MF
- Passamonti et al. developed a prognostic model for post-PV MF patients based on three risk factors (The presence of any of these risk factors results in a 4.2-fold increased risk of death):
- Hemoglobin <100 g/l
- Platelet count <100 × 109/l
- Leukocyte count >30 × 109/l
Compiled by: Dr. Pratyusha Gudapati & Dr. Namrata Kaul
In case of queries, email us at: kumar.ankur@rgcirc.org
Hematolymphoid neoplasm Myeloproliferative neoplasm Polycythemia Vera Post Polycythemia Vera Myelofibrosis
Last modified: 18/06/2021