Background
A 54-year old male, presented with a history of anterior neck swelling, gradually increasing since 1.5 years. CT neck revealed right lobe of thyroid replaced by a heterogeneously hyper-enhancing mass 12.5 x 7.5 x 4cm with multiple right sided cervical lymphadenopathy. S. calcitonin levels were 9.36 pg/ml. FNAC was done from right thyroid lobe. Patient underwent total thyroidectomy with removal of neck nodes.
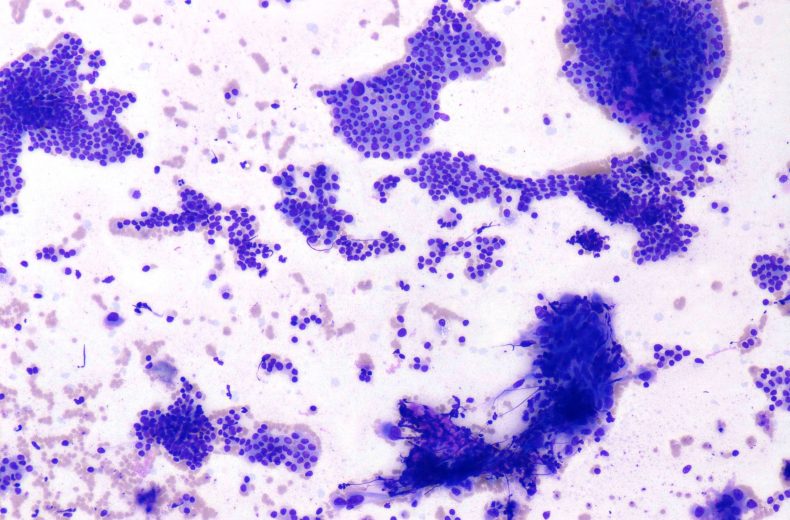
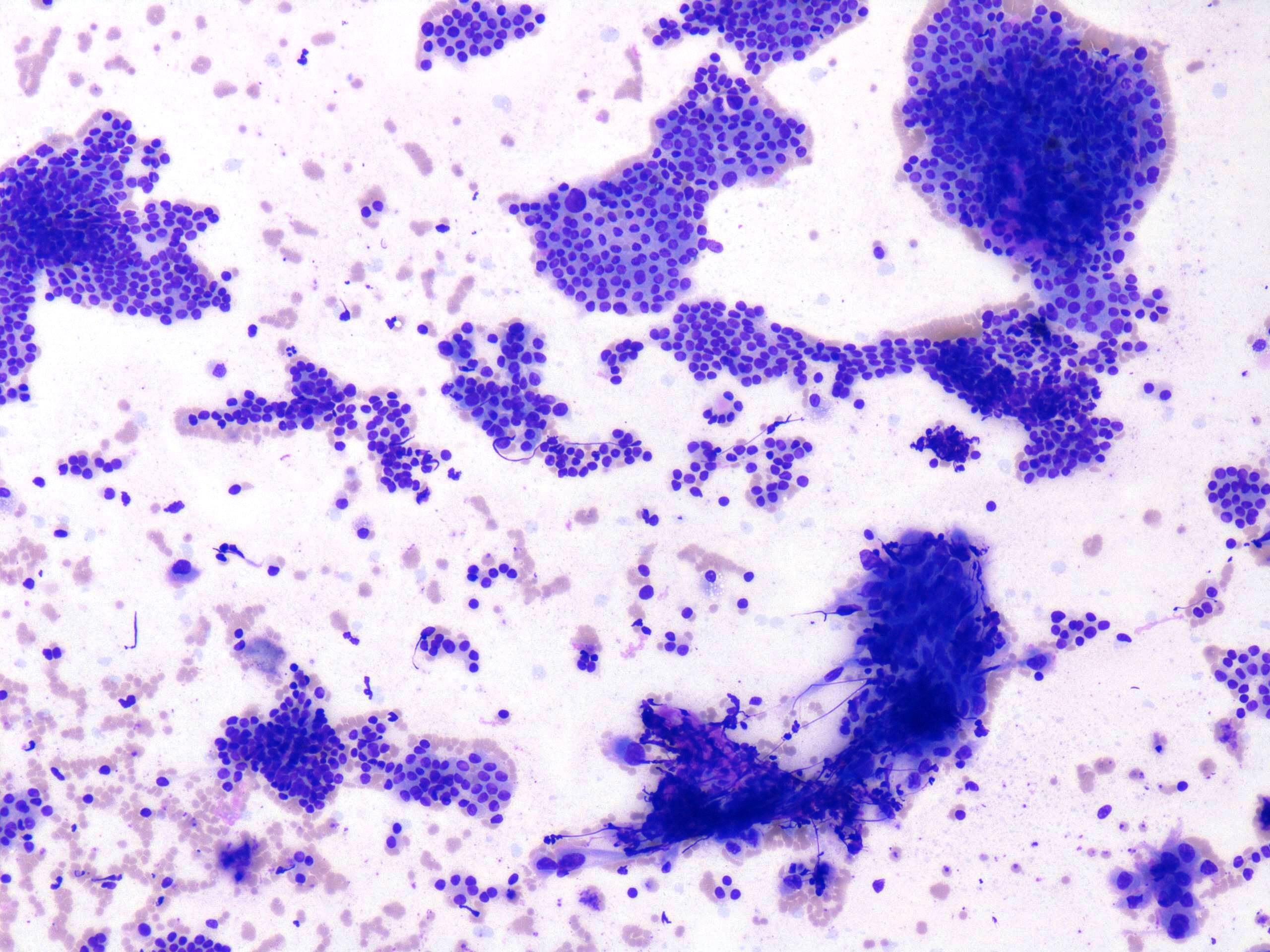
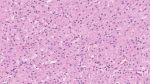
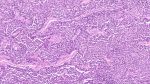
FNAC Smears
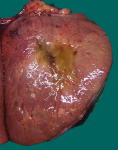
Gross specimen
Fig. 13c-d: Gross examination shows a solid grey white to yellowish mass in right thyroid lobe.
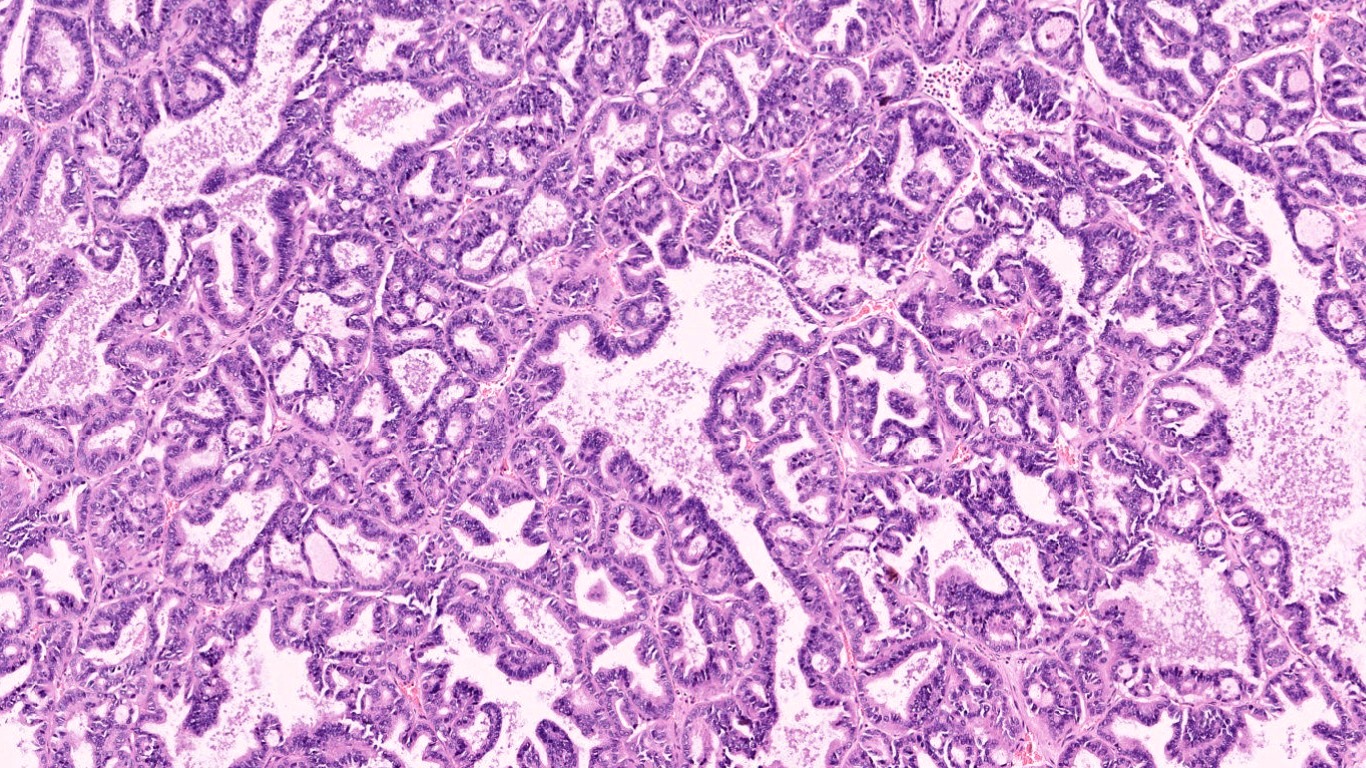
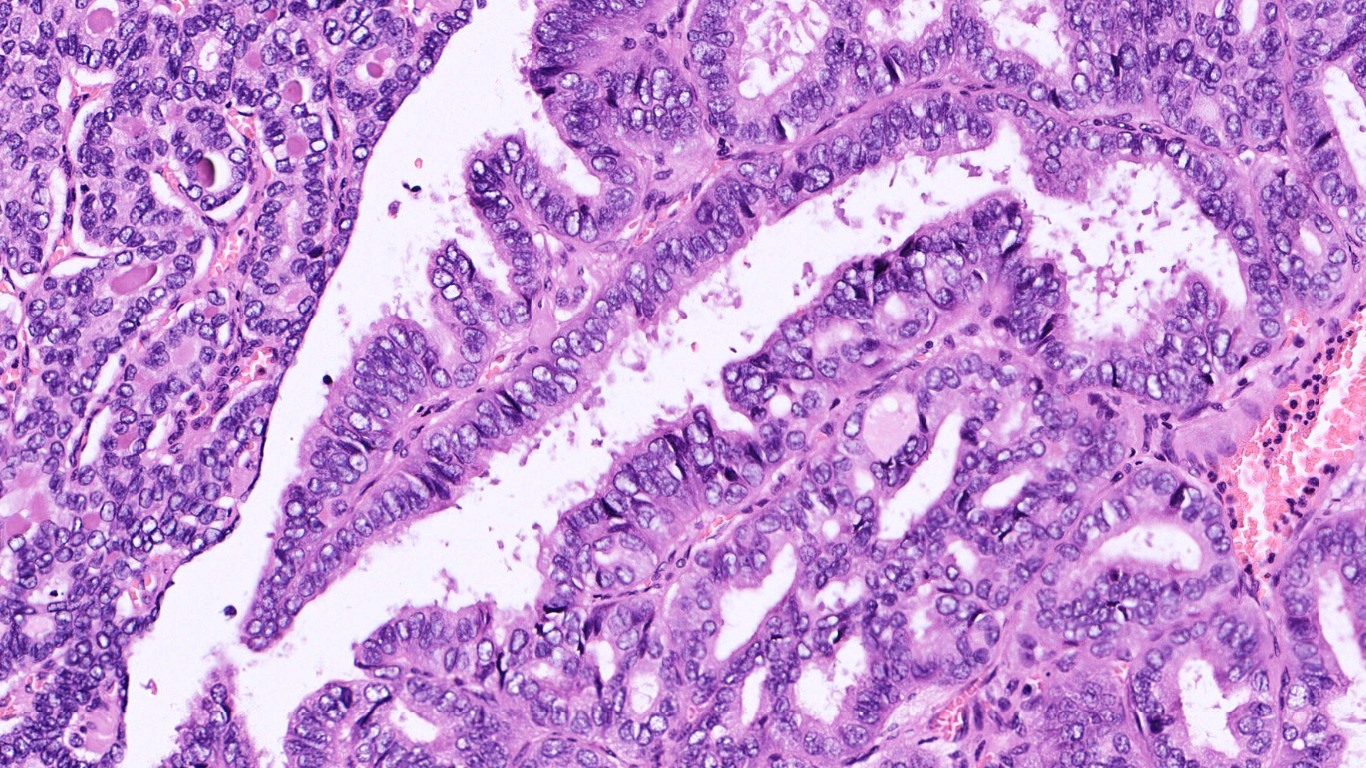
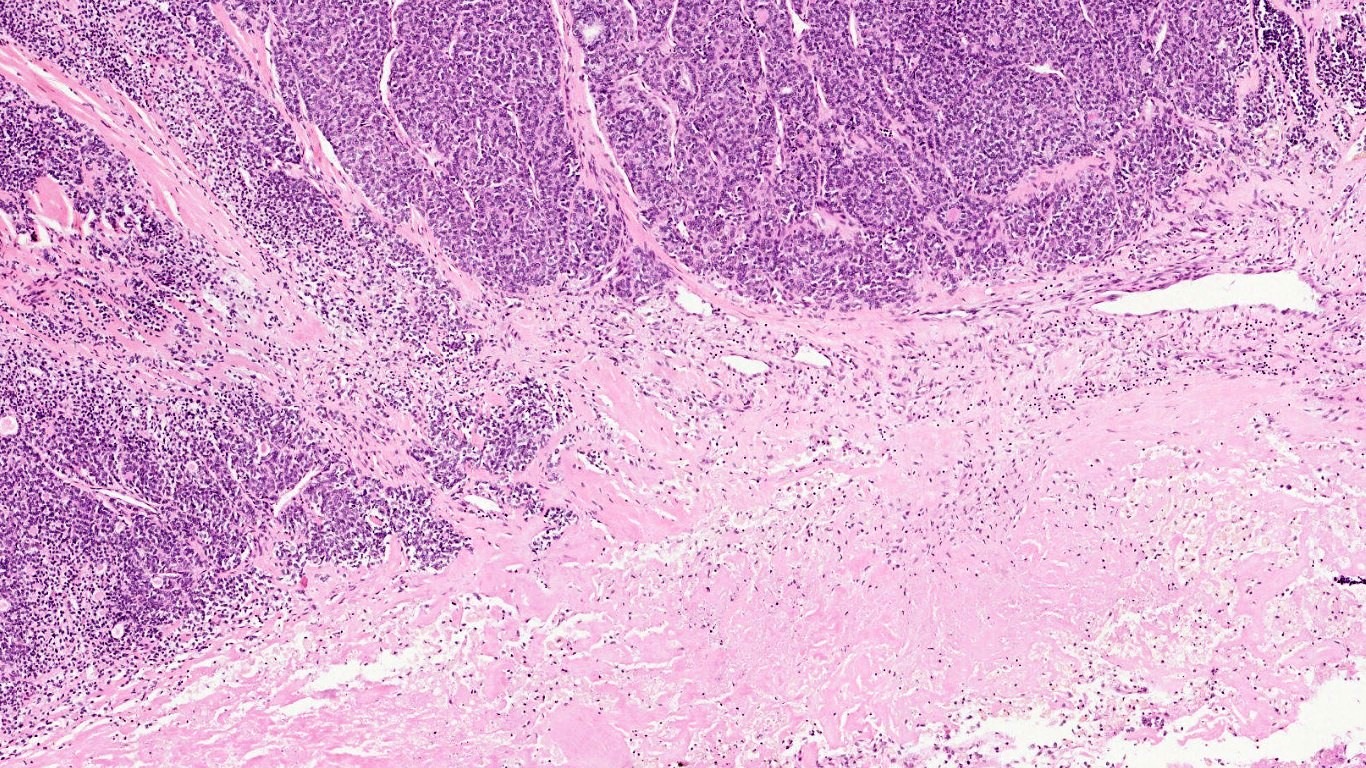
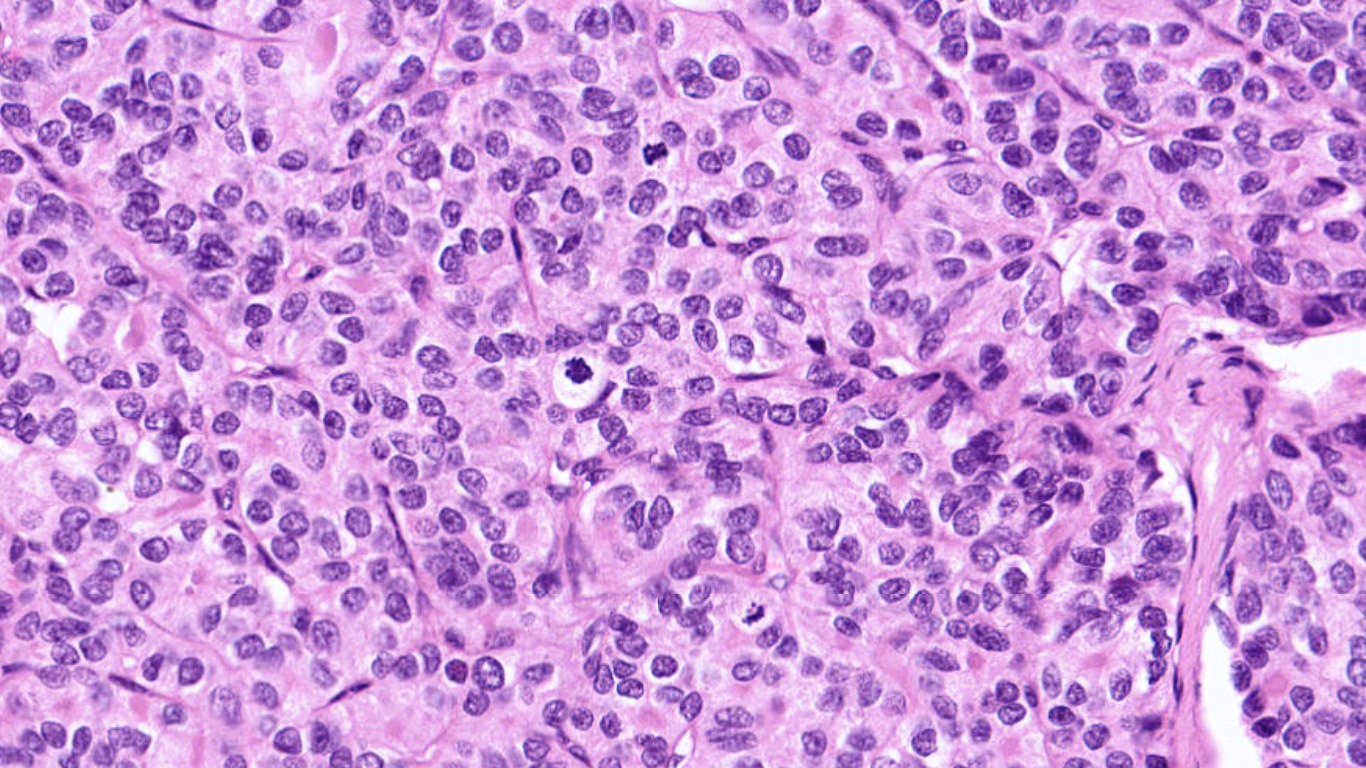
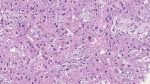
Microscopy
Questions & Answers:
- What is your diagnosis?
- Anaplastic Thyroid Carcinoma
- Papillary Thyroid Carcinoma
- Medullary Thyroid Carcinoma
- Poorly Differentiated Thyroid Carcinoma (with coexistent Papillary Thyroid Carcinoma)
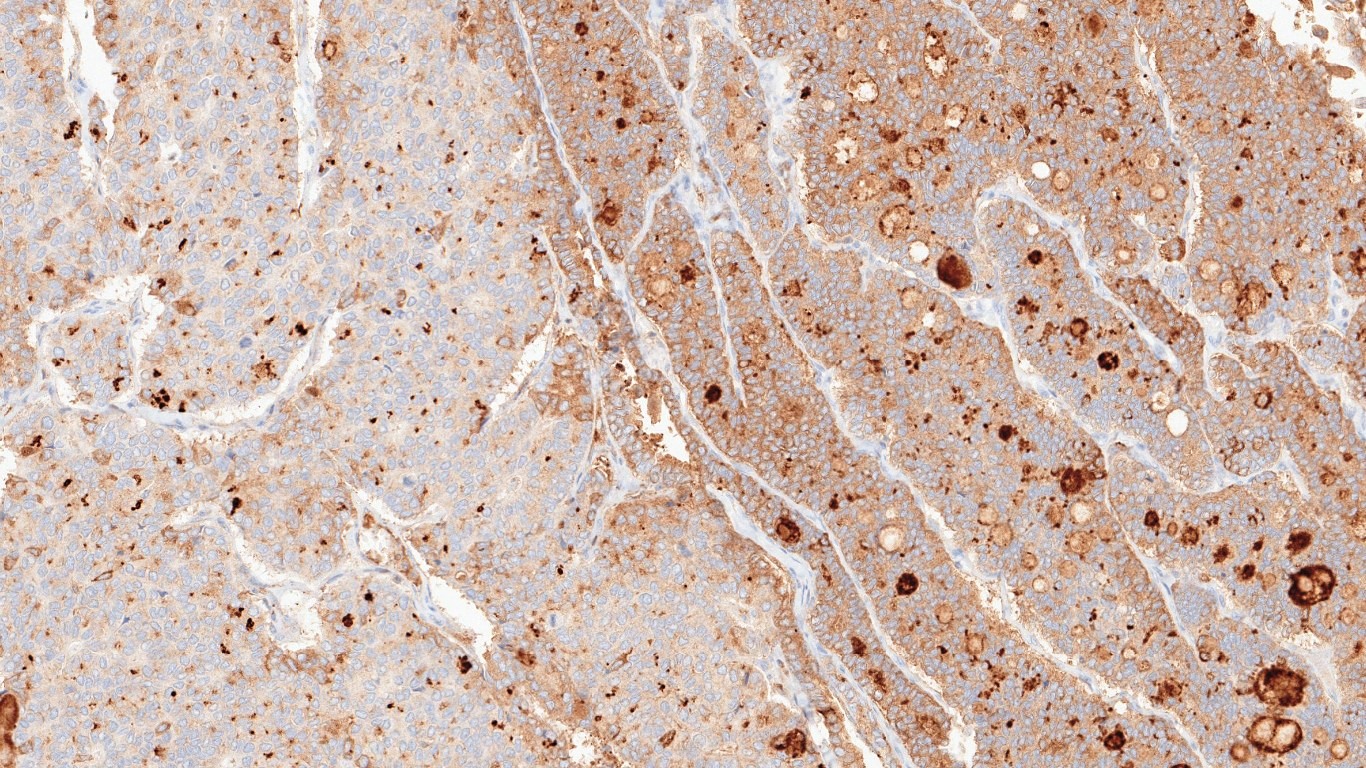
- Which of the following Immunohistochemical (IHC) marker is shown in Fig. 13m?
- PAX8
- TTF1
- Thyroglobulin
- Cytokeratin
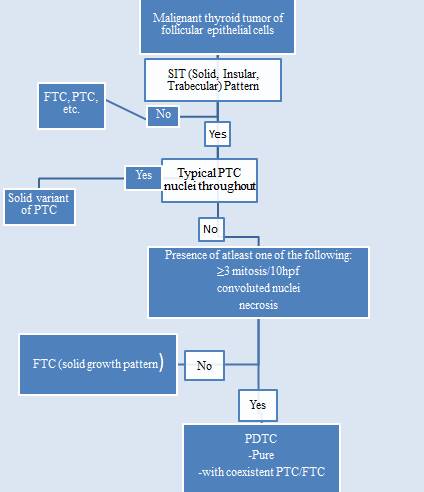
- What is the name of the diagnostic algorithm for this tumor, which is now accepted and integrated in the WHO classification?
- MSKCC criteria
- Turin Consensus Proposal
- ATA guidelines
- AMES criteria
- The term “poorly differentiated thyroid carcinoma” (PDTC) was first introduced by Granner and Buckwalter in the early 1960.
- However, World Health Organization (WHO) series of malignant human neoplasms, first accepted and introduced this entity in 2004.
- Morphologically and biologically, this tumor is placed between well differentiated thyroid carcinoma (PTC, follicular thyroid carcinoma (FTC)) and anaplastic thyroid carcinoma.
- Clinical Features:
- Mean patient age at diagnosis: 55-63 years
- Clinical presentation: Usually large solitary thyroid mass. Distant metastasis at presentation is reported in 15% of cases.
- Tumor spread and staging: Widely invasive into perithyroidal soft tissue, regional lymph nodes and distant metastasis (most commonly, lung followed by bones and other sites). Higher pTNM than well-differentiated thyroid carcinomas.
- Fine-needle Aspiration:
- Challenging owing to their rareness, overlapping morphology with follicular neoplasms and sampling error of the poorly differentiated component.
- Most of the cases are reported as suggestive of follicular neoplasm.
- Cytological features most predictive of PDTC are: severe crowding, clusters with solid/insular architecture, single cells, high N:C ratio and mitotic activity.
- Diagnostic Algorithm for the diagnosis of PDTC using Turin consensus criteria:
- How much poorly differentiated component is needed to call it PDTC?
- Even PDTC component as little as 10% of an otherwise well differentiated tumor, may be associated with aggressive features or have unfavourable prognosis.
- Immunophenotype:
- General features intermediate between well differentiated and anaplastic thyroid carcinomas. No specific marker is diagnostic of PDTC.
- Genetic Profile:
- Early driver events in thyroid carcinogenesis: RAS family, BRAF mutations & ALK fusions
- Late events associated with tumor dedifferentiation: TP53, TERT, CTNN1, AKT1 mutations
- However, there is a vast overlap of mutations in the different subtypes and the lack of specific mutations.
- miR-221 and miR-222 are increasingly deregulated in PDTC as compared with PTC
- Prognosis:
- Overall 5-year survival 60-70%
- The relapse-free survival is less than 12 months
- Treatment:
- No standardized treatment for PDTC to date.
- More aggressive approach is needed to treat these tumors as compared with standard low-risk thyroid carcinomas.
- Response to radioiodine treatment is generally poor.
- Tyrosine kinase inhibitors offer new treatment options in these very difficult to treat tumors.
- Sorafenib and Lenvatinib were approved by the U.S. Food and Drug Administration (FDA) for patients with radioiodine-resistant progressive, recurrent, or metastatic disease.
Contributed & Compiled by: Dr Divya Bansal
In case of queries, email us at: divya.bansal@rgcirc.org
Head & Neck Neoplasms Poorly differentiated thyroid carcinoma Thyroid Turin Consensus Proposal
Last modified: 11/07/2021